Writing a nursing care plan requires much more than simply summarizing a patient’s condition. It involves critical thinking, accurate nursing diagnoses, prioritizing patient needs, planning effective interventions, documenting measurable outcomes, and ensuring evidence-based practice. For many nursing students, the challenge lies in bridging the gap between theory and real-world application, often making the process feel overwhelming. This comprehensive guide is written to support you at every stage of writing a nursing care plan, providing clear step-by-step instructions, practical examples, and ready-to-use templates. Whether you’re a beginner or looking to refine your skills, this guide will make your care plan writing easier, precise, and more effective, helping you excel in academics.
What is a Nursing Care Plan?
A nursing care plan is a structured document that outlines a patient’s current health condition, nursing diagnoses, prioritized needs, and the interventions required to support treatment, recovery, and holistic care. It serves as both a guide and a communication tool, helping nurses set measurable goals, track patient progress, and ensure evidence-based practice. By following a standardized framework, nursing care plans promote collaboration among healthcare professionals, support patient-centered outcomes, and provide a clear record of the nursing process from assessment to evaluation.
How many Types of Nursing Care Plans?
Nursing care plans are generally classified into two main categories: Informal and Formal. Formal care plans can then be further divided into two subtypes: Standardized, which address common needs across groups of patients, and Individualized, which are tailored to meet the unique needs of a single patient.
1. Informal Care Plans
Definition:
An informal nursing care plan is a mental strategy consisting of the nurse’s thoughts, goals, and intended actions for patient care, which remain in the nurse’s mind rather than being formally documented in writing.
Characteristics:
- Unwritten and flexible, existing only in the nurse’s thoughts.
- Focuses on immediate decisions and actions during a shift.
- Guides care in real time without formal documentation.
2. Formal Care Plans
Definition:
A formal nursing care plan is a written or digital document that systematically organizes and coordinates patient information, outlining care strategies based on the individual’s assessed needs.
Characteristics:
- Provides a clear framework for care delivery.
- Updated regularly to reflect patient progress or changing conditions.
- Enhances consistency, accountability, and communication among the care team.
Now, formal care plans are further divided into two main categories: Standardized Care Plans and Individualized Care Plans.
Standardized Care Plans
Definition: A pre-developed formal plan designed for patients with similar health conditions, diagnoses, or needs.
Characteristics:
- Offers consistent, evidence-based care guidelines for groups of patients.
- Saves time and ensures quality by addressing common clinical scenarios.
Individualized Care Plans
Definition: A tailored care plan created for one specific patient, based on their unique health status, needs, and circumstances.
Characteristics:
- Developed after a detailed assessment of the patient.
- Provides personalized interventions and measurable goals.
- Ensures truly patient-centered care.
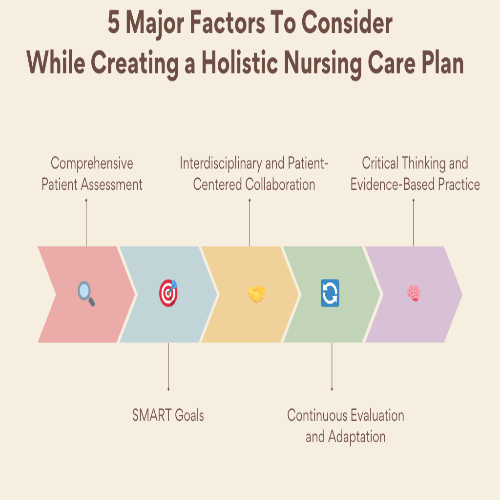
How to Write a Nursing Care Plan?
Now that you have explored the different types of nursing care plans, let’s move on to discussing how to write them step by step and effectively.
How to Develop an Informal Care Plan?
An informal care plan isn’t documented but exists in the nurse’s thought process, requiring more than just intuition. It involves a rapid yet structured mental process that aligns with the nursing frameworks like Orem's Self-Care Deficit Theory, Roy's Adaptation Model, Watson's Theory of Caring, and Peplau's Interpersonal Relations Model. You/nurse, should quickly assess the patient, identify pressing problems, set short-term goals, plan immediate interventions, and evaluate progress throughout the shift. Although this process is not formally documented, it ensures that patient care remains safe, systematic, and responsive.
Here are the steps to follow while developing an informal nursing care plan in your mind:
1. Quick Patient Assessment (Assessment Phase)
Begin by rapidly collecting essential patient data through direct observation and interaction. This includes vital signs, behavior, physical appearance, cognitive state, emotional cues, and environmental risks. For example, a post-operative patient presenting as anxious, diaphoretic, guarding their abdomen, with a respiratory rate of 26, BP of 150/95, and a call bell out of reach, gives immediate clues about potential pain, anxiety, and safety concerns.
This mirrors the Assessment phase of the nursing process and aligns with ANA Standard 1: Assessment, which emphasizes the collection of comprehensive data pertinent to the patient’s health or situation.
2. Problem Identification (Diagnosis Phase)
Synthesize the assessment data to formulate one or more priority nursing diagnoses. Drawing from NANDA-I, identify key problems such as:
- Acute Pain related to surgical trauma, evidenced by guarding and elevated vitals
- Anxiety related to an unfamiliar environment and post-op status
- Risk for Injury (Falls) related to impaired mobility and environmental hazards (e.g., call bell out of reach)
This diagnostic reasoning corresponds with ANA Standard 2: Diagnosis and reflects critical thinking guided by evidence-based classification systems.
3. Set Immediate, Shift-Level Goals (Planning Phase)
Establish short-term, achievable goals that can be addressed during your shift. Use the SMART criteria (Specific, Measurable, Achievable, Relevant, Time-bound) to frame expected outcomes. For example:
- “Patient’s pain will reduce to ≤3/10 within 1 hour after analgesic administration.”
- “SpO₂ will remain ≥92% on 2L O₂ by nasal cannula.”
- “Patient will demonstrate use of the call bell and maintain a safe environment during the shift.”
These goals address Maslow’s physiological and safety needs, placing pain control and safety as foundational priorities.
4. Plan Mental Interventions (Implementation Phase)
Choose appropriate, real-time interventions that directly support the goals. Even without documentation, your actions should reflect evidence-based practice. For this patient:
- Elevate the head of the bed to ease breathing
- Administer prescribed analgesia
- Apply oxygen as ordered.
- Reposition the call bell within reach and instruct the patient in its use..
- Offer brief emotional support and guide the patient through pursed-lip breathing
This step corresponds with ANA Standard 5A: Implementation and aligns with Orem’s Self-Care Deficit Theory, as you're temporarily compensating for what the patient cannot manage independently.
5. Continuous Monitoring & Adaptation (Evaluation Phase)
Closely observe the patient’s response and adapt your care in real time. This aligns with Roy’s Adaptation Model, which views the patient as a dynamic system responding to internal and external stimuli. For instance:
- If pain reduces to 3/10 but respiratory rate remains high, you might reassess anxiety and consider further calming techniques.
- If SpO₂ improves but the patient appears drowsy, evaluate for over-sedation or other complications.
This reflects ANA Standard 6: Evaluation, ensuring continuous, reflective practice.
6. Foundation for Formal Documentation
Although initiated informally, this care process provides a strong base for structured documentation. The diagnoses, interventions, and observed responses can later be entered into the formal care plan. For example, this case may be formally documented under:
- NANDA-I Diagnosis: Acute Pain, Anxiety, Risk for Injury
- Interventions: Oxygen therapy, positioning, reassurance, pain management
- Evaluation: Goals met (e.g., SpO₂ ≥92%), partially met (e.g., patient still anxious with exertion)
This supports continuity of care and complies with ANA Standard 10: Documentation, reinforcing legal and ethical standards of practice.
By integrating these steps into your thought process, you can craft an informal care plan that is flexible, patient-centered, and responsive, ensuring quality care even when documentation is not immediately possible.
How to develop the Formal Nursing Care Plan?
Now that you understand how informal care plans work, it’s important to know that not all care plans are undocumented. Many situations require a formal nursing care plan, a written or computerized document created using structured templates. Formal plans are carefully documented to ensure clarity, accountability, and communication across the healthcare team. They not only guide patient care but also serve as a legal and professional record of nursing practice.
Now, let us discuss how to write an effective formal nursing care plan step by step:
Clinically Relevant Assessment Data
Begin by collecting all clinically relevant information that forms the foundation of your care plan. This includes vital signs, reported symptoms, medical history, and key lab findings. For example, a patient with a known history of chronic obstructive pulmonary disease (COPD) presents with a respiratory rate of 24 breaths/min, heart rate of 110 bpm, SpO₂ of 92%, and complaints of chest pain and shortness of breath. Arterial blood gases (ABG) reveal mild hypoxia with a PaO₂ of 70 mmHg. These findings collectively highlight both physiological and clinical indicators that require prompt nursing attention. This step aligns with the Assessment phase of the nursing process (ANA Standard 1).
Cluster of Assessment Data for Nursing Diagnosis
Organize and group your assessment data into clusters that point toward a specific nursing problem. By identifying related symptoms and signs, you can clearly define the issue. In this case, the patient’s elevated respiratory rate, use of accessory muscles, decreased SpO₂, exertional chest pain, and reports of dyspnea form a clear cluster supporting the nursing diagnosis of Ineffective Breathing Pattern. This reflects the Diagnosis phase, where data is analyzed to identify patient problems.
Defining Characteristics for Nursing Diagnosis
List the observable cues and patient-reported experiences that confirm the presence of the identified problem. For an Ineffective Breathing Pattern, defining characteristics include tachypnea, visible use of accessory muscles during inspiration, oxygen saturation of 92%, and shortness of breath with minimal exertion. The patient’s COPD history adds important clinical context, increasing vulnerability to respiratory complications. This step helps justify your diagnosis with concrete evidence.
Nursing Interventions
Develop specific, actionable interventions that directly address the nursing diagnosis. These should be individualized and clearly stated. For this patient:
- The nurse will administer oxygen at 2L/min via nasal cannula to maintain SpO₂ above 92%.
- The nurse will assist the patient into a high Fowler’s position to promote optimal lung expansion.
- The nurse will monitor respiratory rate, SpO₂, and use of accessory muscles every 2 hours to track respiratory status and effectiveness of interventions.
This corresponds to the Implementation phase, where planned nursing actions are carried out.
Rationale for Each Intervention
Provide an evidence-based justification for each intervention to ensure clarity and align with best practices. Administering low-flow oxygen helps improve oxygenation and reduce breathing effort in COPD patients, as recommended by the American Thoracic Society (2020) guidelines. Upright positioning enhances diaphragmatic movement and lung capacity, relieving respiratory distress. Regular monitoring enables timely detection of changes, allowing adjustments to care as needed. This explanation supports the interventions with a scientific rationale.
Evaluation
Assess whether expected outcomes were achieved using clinical data and patient feedback. Use criteria like Met, Partially Met, or Not Met. For example, the goal of maintaining SpO₂ ≥ 92% was met: the patient’s saturation improved to 94% after oxygen therapy, respiratory rate decreased to 20 breaths/min, and accessory muscle use was no longer evident. The patient also reported less shortness of breath. This critical step mirrors the Evaluation phase, ensuring care effectiveness.
Revision of Plan
If goals are partially met or unmet, revise your care plan accordingly. For instance, if SpO₂ remains borderline at 92% and accessory muscles are still used during ambulation, update the plan by increasing oxygen to 3L/min and rechecking saturation in 1 hour. Adding deep breathing exercises every 2 hours can promote lung expansion and reduce accessory muscle reliance. This step emphasizes the dynamic, ongoing nature of nursing care planning.
This step-by-step approach, grounded in the nursing process theory and guided by professional standards, ensures your formal nursing care plan is clear, structured, and focused on achieving positive patient outcomes. By following this format, you address every essential component, from assessment to evaluation, while using evidence-based practices to tailor your interventions effectively.
Subtypes:
Standardized Nursing Care Plan
A standardized nursing care plan uses predefined elements, nursing diagnoses, interventions, goals, and evaluations to streamline care delivery while maintaining flexibility for patient-specific needs. This type of plan is particularly useful for commonly encountered clinical problems such as impaired breathing, risk for falls, or pain management.
1. Diagnosis
Begin by clearly stating the nursing diagnosis, using standardized language (e.g., NANDA-I terminology). This ensures your diagnosis is both clinically sound and supported by evidence-based guidelines.
In the case of a patient with COPD experiencing shortness of breath, use of accessory muscles, and a SpO₂ of 92%, a relevant diagnosis might be:
Diagnosis: Ineffective Breathing Pattern related to alveolar-capillary membrane changes and increased work of breathing as evidenced by tachypnea, use of accessory muscles, and reduced oxygen saturation.
2. Goals / Expected Outcomes
Next, establish clear, measurable, and time-bound goals following the SMART framework (Specific, Measurable, Achievable, Relevant, Time-bound). These outcomes define what success looks like for this patient and provide benchmarks for evaluation.
For our COPD patient:
- Goal 1: Patient will maintain SpO₂ at or above 94% on supplemental oxygen within 4 hours.
- Goal 2: Patient will report decreased shortness of breath and demonstrate a relaxed breathing pattern within 8 hours.
3. Nursing Interventions
Select evidence-based, standardized interventions appropriate for the patient’s condition. These actions should be stated in direct, action-oriented language and tailored to the patient’s clinical status.
For this patient with an Ineffective Breathing Pattern, interventions may include:
- The nurse will administer oxygen at 2L/min via nasal cannula and titrate per protocol to maintain target saturation.
- The nurse will assist the patient into high Fowler’s position to enhance diaphragmatic excursion and lung expansion.
- The nurse will monitor respiratory rate, use of accessory muscles, and SpO₂ every 2 hours.
- The nurse will teach the patient pursed-lip breathing techniques to promote controlled exhalation and reduce air trapping.
4. Evaluation
Assess the patient’s progress in relation to the established goals. Determine whether each goal is Met, Partially Met, or Not Met, using both objective and subjective data.
For our COPD case:
- Goal 1: Met, Patient’s SpO₂ increased to 94% within 3 hours on 2L O₂, maintained for 4 consecutive hours.
- Goal 2: Partially Met, Patient reports less shortness of breath and demonstrates use of breathing techniques, but still requires support during exertion.
Common Formats for Standardized Nursing Care Plans
1. Four-Column Table Layout
This is the most widely used format in clinical settings. It offers a structured, easy-to-follow flow of information.
Diagnosis | Goals/Expected Outcomes | Nursing Interventions | Evaluation |
Ineffective Breathing Pattern | Patient will maintain SpO₂ ≥94% within 4 hours. | Administer oxygen at 2L/min and position the patient upright. | Met: SpO₂ stabilized at 94% after 3 hours. |
Patient will demonstrate improved breathing pattern by the end of the shift. | Teach pursed-lip breathing and monitor respiratory effort q2h. | Partially Met: Breathing technique used, but SOB persists during ambulation. |
2. Three-Column Format
This simplified format combines goals and evaluation into one column, making it ideal for fast-paced environments or electronic documentation systems.
Diagnosis | Interventions | Outcomes / Evaluation |
Ineffective Breathing Pattern | Administer oxygen, elevate the head of the bed, and teach breathing exercises. | Met: SpO₂ maintained ≥94%; Partially Met: SOB decreased but is still present with activity. |
3. Five-Column Format
Used in academic or high-detail settings, this layout includes Assessment and Rationale, offering a deeper clinical rationale for each component of the plan.
Assessment | Diagnosis | Goals/Expected Outcomes | Nursing Interventions | Rationale/Evaluation |
RR 24, HR 110, SpO₂ 92%, accessory muscle use, patient reports SOB | Ineffective Breathing Pattern | Maintain SpO₂ ≥94% within 4 hours; improve respiratory comfort by end of shift | Administer oxygen at 2L/min, assist to high Fowler’s, teach pursed-lip breathing.. | Oxygen improves gas exchange; upright posture optimizes lung expansion; breathing techniques reduce air trapping. SpO₂ improved to 94%; SOB reduced. |
Why This Structure Works for Standardized Care Plans
- Consistency: Using standardized diagnoses and interventions ensures that care delivery is consistent across similar patient populations, improving quality and reliability.
- Efficiency: Predefined frameworks save time without sacrificing quality, especially for frequently encountered problems like ineffective breathing, fall risk, or impaired mobility.
- Documentation Quality: Structured formats ensure all critical elements, diagnosis, interventions, goals, and evaluation are documented clearly, improving communication, continuity of care, and audit readiness.
Summary: Key Takeaways
- The four-column format balances clarity and detail, making it ideal for most clinical documentation.
- The three-column layout is perfect for quick charting and efficiency in time-sensitive settings.
- The five-column format adds academic depth, useful for nursing students, care plan evaluations, or complex patient scenarios.
By following a standardized care planning approach with embedded evidence and clear structure, you ensure that patient care is efficient, consistent, and tailored, all while aligning with professional standards and best practices.
Individualized Nursing Care Plan
An individualized nursing care plan (INCP) uses the ADPIE nursing process (Assessment, Diagnosis, Planning, Implementation, Evaluation) to address a patient’s unique needs, strengths, preferences, and goals. This plan guides both the patient and healthcare team toward improved outcomes and satisfaction.
1. Nursing Diagnosis
Identify the nursing diagnosis based on thorough assessment data. Use NANDA-I terminology but tailor it to the patient’s specific condition.
Example:
Diagnosis: Acute Pain related to surgical incision (following abdominal surgery).
2. Goals / Expected Outcomes
Set personalized, SMART goals that are time-bound, achievable, and aligned with the patient’s values and preferences. Collaborate with the patient and family to ensure goals reflect their priorities.
Example:
- Goal 1: Patient will report pain ≤ 3/10 within 1 hour using the agreed pain relief method.
- Goal 2: Patient will use preferred relaxation techniques (e.g., guided imagery with familiar music) to manage pain within 24 hours.
3. Interventions
List specific, patient-centered interventions tailored to the patient’s abilities, preferences, cultural background, and resources. Involve the patient and family in planning to ensure relevance.
Example:
- Administer as-needed analgesic based on the patient’s previous positive response.
- Incorporate cultural preference by applying a warm compress to the incision site.
- Encourage deep breathing exercises with music or guided imagery that resonates with the patient.
- Educate the patient about pain management techniques, emphasizing preferred methods.
4. Evaluation & Revisions
After interventions, evaluate the patient’s progress toward goals. Document whether goals are Met, Partially Met, or Not Met. Use findings to revise and update the care plan as needed for ongoing relevance and effectiveness.
Example:
- Evaluation 1: Met, Patient reported pain 2/10 after analgesic and warm compress.
- Evaluation 2: Met, Patient used guided imagery with personal music, reported calm breathing, and reduced pain.
- Revision: Continue current pain management methods and assess for any new comfort needs as recovery progresses.
Why This Format Works for Individualized Care Plans
- Personalized Care: Ensures the plan reflects the patient’s unique needs, values, and preferences.
- Patient Engagement: Involving patients and family in goal-setting improves adherence and outcomes.
- Adaptability: The dynamic nature allows updates based on patient response and changing needs.
- Continuity of Care: A Structured approach improves communication and clarity across care teams.
Practical Example: Individualized Nursing Care Plan for "Acute Pain"
Diagnosis | Acute Pain related to surgical incision |
Goals / Expected Outcomes | 1. Patient will report pain ≤ 3/10 within 1 hour using the agreed pain relief method. |
2. Patient will use preferred relaxation technique (guided imagery with familiar music) within 24 hours. | |
Interventions | 1. Administer as-needed analgesic based on the patient’s prior positive response. |
2. Apply a warm compress, respecting the patient’s cultural preferences. | |
3. Encourage deep breathing exercises with music or guided imagery. | |
Evaluation & Revisions | Met: Patient reported pain 2/10 after analgesic and warm compress. |
Met: Patient used guided imagery with personal music and reported calm breathing. | |
Revision: Continue current pain management; assess for new comfort needs. |
Summary Table: Key Components
Format Element | Description |
Diagnosis | Based on NANDA-I but tailored to the patient’s specifics. |
Goals/Expected Outcomes | Personalized SMART goals reflecting patient priorities. |
Interventions | Customized, evidence-based actions respecting patient preferences. |
Evaluation & Revisions | Continuous assessment and plan updates to maintain effectiveness. |
An individualized nursing care plan combines the structure of ADPIE with flexibility, focusing on holistic, patient-centered care. It evolves with the patient’s changing needs, ensuring care remains effective and relevant for the best possible outcomes.
Conclusion:
Ultimately, writing a nursing care plan is a crucial skill that requires a deep understanding of both theoretical knowledge and practical application. By following a structured approach, whether developing an informal, formal, standardized, or individualized care plan, nurses ensure that patients receive comprehensive, individualized care that addresses their unique needs, preferences, and goals. The process involves careful assessment, clear nursing diagnoses, targeted interventions, and ongoing evaluation, all based on evidence-based practice.
A well-crafted nursing care plan not only guides care delivery but also promotes effective communication among the healthcare team, ensuring that each team member is aligned with the patient's evolving condition and needs. It provides a valuable tool for improving patient outcomes, enhancing satisfaction, and reducing the risks of errors or missed interventions.
Whether you're a beginner or looking to refine your skills, mastering the art of writing nursing care plans will empower you to provide high-quality, patient-centered care. However, by incorporating the steps outlined in this guide, you can confidently navigate the complexities of care planning and contribute to better clinical decision-making and improved patient outcomes.